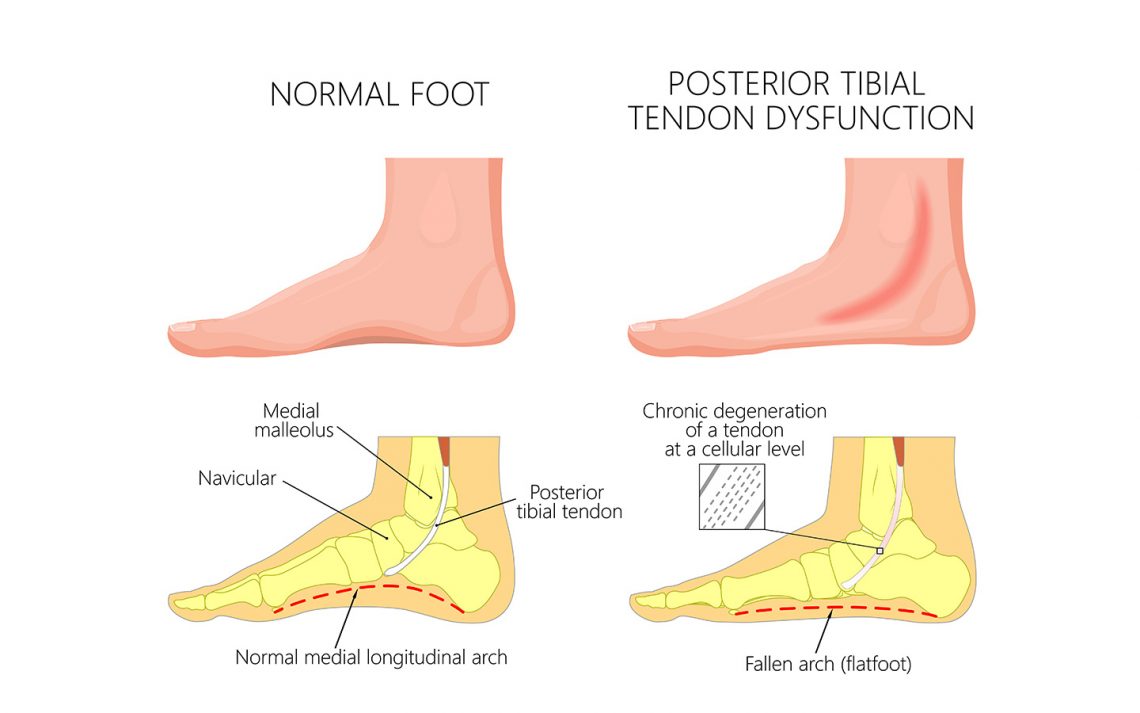
Posterior Tibial Tendon Dysfunction (PTTD) is one of the most common tendinopathies of the foot, which can also lead to adult acquired flat foot deformity if left untreated.

What causes PTTD?
The most common cause of PTTD is increased demand on the posterior tibial tendon and accompanied by elongation of the tendon. There is usually pain, irritation, inflammation and swelling in the medial ankle and arch of the foot but also along the tendon line.
What affects tendon load demands?
Firstly, we need to understand the basic science of tendons and how they work. Tendon structure, mechanical properties, anatomical position and geometry play a role in adult acquired flat foot deformity. Below we analyse some of these aspects, in relation to foot posture and posterior tibial tendon demands.
Structure
Tendons are soft tissues that connect muscles to bone and are responsible for guiding and share load amongst the joints. There are many building blocks that make up tendons and other soft tissues in the body. Tendons are typically formed of Type-I collagen, which makes up around 70-80% and provide its tensile strength. Tensile strength is how strong a structure is when it is being pulled apart or an attempt to “stretch it out”. Also around 1% is elastin and other forms of collagen, glycans and proteoglycans, which are responsible for the viscoelasticity properties of the tendon, which means how easy they are to return to the original length once it is no longer being stretched. In essence, collagen fibrils connect into bundles whereby bundle after bundle eventually make up the tendon (collagen molecules>fibrils>fibres>fascicles>tendon unit). The larger the diameter of the tendon the greater is the resistance to stress and therefore ability to withstand greater demands, just like a thick rope will be able to pull up a greater amount of weight.
Stress v. Strain
As the tendon is put under stress (pull motion) it is then elongated (strain) (Fig.1).
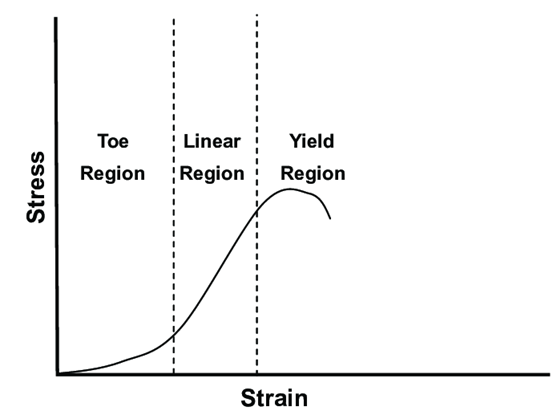
(Fig.1 Stress v. Strain curve)
The viscoelasticity properties of tendons allows them to recoil back to their original resting position once the load is removed, however, if the tendon is being pulled apart long enough it then experiences something called creep and stress relaxation (Fig.2).
This happens when tendon plasticity is lost and permanent elongation occurs as a result. The loss of this ability from the posterior tibial tendon to return to its original length is common in severe cases of PTTD.
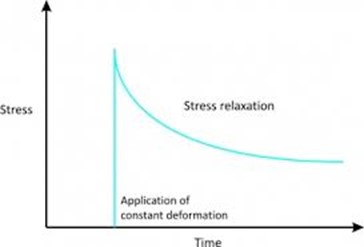
(Fig.2 Stress Relaxation)
In extreme cases for example if the tendon is stressed beyond its limit, it will eventually fail and rupture and in the case of PTTD fixed deformity to occur.
Subtalar joint and knee joint alignment
The subtalar joint is considered responsible for the side-to-side movement of the foot. Each tendon has an origin and an insertion or attachment point. Where the tendon attaches usually dictates the motion of a particular joint. There are muscles on either side of the subtalar joint that act either to pull in or pull out the foot. Because of the location of the posterior tibial tendon insertion it is responsible to invert the foot (pull the foot inwards) and during walking to support the medial longitudinal arch of the foot (Pic. 1) as it accepts the weight of the walking person. The more lateral heel placement in a pronated foot creates an extrinsic force that drives the foot further into pronation and into a vicious cycle. In a severely collapsed arch, the tendon is put under enormous strain and the load demands are high, therefore the resistance to reduce these load demands are high (Pic.2).
Knee position – valgus knees, which are usually associated with a valgus foot can also increase this load as the load line through the knee falls medially thereby having a similar effect.

(Pic.2)
How can we describe PTTD?
It is typically described in 4 stages depending on severity and there are clinical findings to allow clinicians to differentiate in each stage.
How do we manage or treat PTTD?
A walking boot can be used to immobilise the foot and relieve pain followed by the use of orthotic inserts to support the foot. Reduction in activity to offload the foot and canes may also be used if appropriate. Materials and characteristics of the orthotic can influence the demands on the stretched tendon and usually have an aggressive design. Biomechanically they aim to reduce the extrinsic pronatory forces and reduce the strain the tendon undergoes. Appropriate footwear that are supportive and can “hold” the foot are desirable thereafter and long term.
Surgery is an option when conservative management options fail and usually involve a rearfoot reconstruction to rebalance the demands on the foot structures.
